Overview
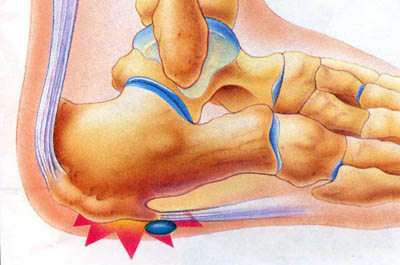
Between the heel bone and the plantar fascia is a small fluid filled sac that is called the plantar (bottom of) calcaneal (heel bone) bursa. The plantar calcaneal bursa?s job is to allow the plantar fascia to glide easily over the heel bone without irritation. If this becomes inflamed and irritated a plantar calcaneal bursitis occurs which can be extremely painful and disabling forcing the athlete to stop training.
Causes
Inflammation of the bursa causes synovial cells to multiply and thereby increases collagen formation and fluid production. A more permeable capillary membrane allows entrance of high protein fluid. The bursal lining may be replaced by granulation tissue followed by fibrous tissue. The bursa becomes filled with fluid, which is often rich in fibrin, and the fluid can become hemorrhagic. One study suggests that this process may be mediated by cytokines, metalloproteases, and cyclooxygenases.
Symptoms
Below is a list of common signs and symptoms of retrocalcaneal bursitis. Recognizing and treating symptoms early can prevent retrocalcaneal bursitis from becoming chronic. Swelling. The retrocalcaneal bursa is located behind the Achilles tendon, just above where the tendon attaches to the heel bone. When the bursa is inflamed it will cause visible soft tissue swelling near the top of the heel bone. It is worth noting that bursitis of the retroachilles bursa, which is located between the Achilles tendon and skin, can manifest slightly differently: swelling may be more distinct, appearing as a hard lump behind the heel. Retroachilles bursitis is also more likely than retrocalcaneal bursitis to cause the skin at the back of the heel to turn red.
Diagnosis
Bursitis is usually diagnosed after a careful physical examination and a full review of your medical history. If you garden and spend a lot of time on your knees, or if you have rheumatoid arthritis, tell your doctor, this information can be very helpful. During the physical exam, he or she will press on different spots around the joint that hurts. The goal is to locate the specific bursa that is causing the problem. The doctor will also test your range of motion in the affected joint. Other tests usually aren?t required to diagnose bursitis, but your doctor may suggest an MRI, X-ray or ultrasound to rule out other potential causes of pain.
Non Surgical Treatment
Treatments should involve decreasing swelling, relieving pain and stress on the Achilles, correcting any biomechanical dysfunction (over-pronation or flat feet), treating scar tissue, and then restoring strength and movement. If you are performing an activity that could cause further trauma to the bursa, it is recommended that you protect the area with padding and/or proper footwear to prevent further irritation or damage.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
Between the heel bone and the plantar fascia is a small fluid filled sac that is called the plantar (bottom of) calcaneal (heel bone) bursa. The plantar calcaneal bursa?s job is to allow the plantar fascia to glide easily over the heel bone without irritation. If this becomes inflamed and irritated a plantar calcaneal bursitis occurs which can be extremely painful and disabling forcing the athlete to stop training.
Causes
Inflammation of the bursa causes synovial cells to multiply and thereby increases collagen formation and fluid production. A more permeable capillary membrane allows entrance of high protein fluid. The bursal lining may be replaced by granulation tissue followed by fibrous tissue. The bursa becomes filled with fluid, which is often rich in fibrin, and the fluid can become hemorrhagic. One study suggests that this process may be mediated by cytokines, metalloproteases, and cyclooxygenases.
Symptoms
Below is a list of common signs and symptoms of retrocalcaneal bursitis. Recognizing and treating symptoms early can prevent retrocalcaneal bursitis from becoming chronic. Swelling. The retrocalcaneal bursa is located behind the Achilles tendon, just above where the tendon attaches to the heel bone. When the bursa is inflamed it will cause visible soft tissue swelling near the top of the heel bone. It is worth noting that bursitis of the retroachilles bursa, which is located between the Achilles tendon and skin, can manifest slightly differently: swelling may be more distinct, appearing as a hard lump behind the heel. Retroachilles bursitis is also more likely than retrocalcaneal bursitis to cause the skin at the back of the heel to turn red.
Diagnosis
Bursitis is usually diagnosed after a careful physical examination and a full review of your medical history. If you garden and spend a lot of time on your knees, or if you have rheumatoid arthritis, tell your doctor, this information can be very helpful. During the physical exam, he or she will press on different spots around the joint that hurts. The goal is to locate the specific bursa that is causing the problem. The doctor will also test your range of motion in the affected joint. Other tests usually aren?t required to diagnose bursitis, but your doctor may suggest an MRI, X-ray or ultrasound to rule out other potential causes of pain.
Non Surgical Treatment
Treatments should involve decreasing swelling, relieving pain and stress on the Achilles, correcting any biomechanical dysfunction (over-pronation or flat feet), treating scar tissue, and then restoring strength and movement. If you are performing an activity that could cause further trauma to the bursa, it is recommended that you protect the area with padding and/or proper footwear to prevent further irritation or damage.
Surgical Treatment
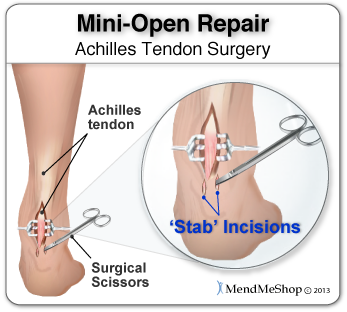
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
 Symptoms
Symptoms Overview
Overview Symptoms
Symptoms Prevention
Prevention A bunion is a firm, painful bump that forms over a bony bulge at the base of the big toe. In most cases, the big toe joint also is enlarged and has degenerative arthritis. The toe also may be pushed toward the second toe (hallux valgus). Bunions tend to be inherited, but they also are common in the following groups. Women who wear high heels. People who wear shoes that are too narrow or too pointed. People with flatfeet. All of these situations force the big toe to drift toward the little toes, and this can cause bunions to form.
A bunion is a firm, painful bump that forms over a bony bulge at the base of the big toe. In most cases, the big toe joint also is enlarged and has degenerative arthritis. The toe also may be pushed toward the second toe (hallux valgus). Bunions tend to be inherited, but they also are common in the following groups. Women who wear high heels. People who wear shoes that are too narrow or too pointed. People with flatfeet. All of these situations force the big toe to drift toward the little toes, and this can cause bunions to form.



 A rupture of the Achilles tendon is one of the more common types of tendon ruptures. As the largest tendon in the human body, the Achilles tendon is very important to one?s balance and stability. Patients who suffer an Achilles tendon rupture experience severe pain and often require Achilles tendon surgery to repair the damage. There are also less invasive methods of Achilles tendon treatment including, icing, anti-inflammatory medications, rehabilitation, taping or bracing, sports massages and more. Achilles tendon recovery is dependent on the health of the patient, and the severity of the injury. Causes Achilles tendon rupture occurs in people that engage in strenuous activity, who are usually sedentary and have weakened tendons, or in people who have had previous chronic injury to their Achilles tendons. Previous injury to the tendon can be caused by overuse, improper stretching habits, worn-out or improperly fitting shoes, or poor biomechanics (flat-feet). The risk of tendon rupture is also increased with the use of quinolone antibiotics (e.g. ciprofloxacin, Levaquin). Symptoms Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people experience pain, possibly severe, and swelling near your heel. An inability to bend your foot downward or "push off" the injured leg when you walk. An inability to stand up on your toes on the injured leg. A popping or snapping sound when the injury occurs. Seek medical advice immediately if you feel a pop or snap in your heel, especially if you can't walk properly afterward. Diagnosis A typical history as detailed above together with positive clinical examination usually will clinch the diagnosis. In an acute rupture, one can usually feel the gap in the tendon from the rupture. There may be swelling or bruising around the ankle and foot of the injured leg. With the patient lying on the tummy (prone position) with the knee flexed, the examiner should see the ankle and foot flex downwards (plantarward) when squeezing the calf muscles. If there is no movement in the ankle and foot on squeezing the calf muscle, this implies that the calf muscle is no longer attached to the heel bone due to a complete Achilles tendon rupture. Non Surgical Treatment Once the Achilles tendon is partially damaged, one should exercise great care. The risk of rupture is high and if pain is associated with walking, one should consult with an orthopedic surgeon or a sports physician. A complete rupture of the Achilles tendon is never treated at home. It is important to understand that there are no minerals, nutrients, or herbs to treat Achilles tendon injury and any delay just worsens the recovery.
A rupture of the Achilles tendon is one of the more common types of tendon ruptures. As the largest tendon in the human body, the Achilles tendon is very important to one?s balance and stability. Patients who suffer an Achilles tendon rupture experience severe pain and often require Achilles tendon surgery to repair the damage. There are also less invasive methods of Achilles tendon treatment including, icing, anti-inflammatory medications, rehabilitation, taping or bracing, sports massages and more. Achilles tendon recovery is dependent on the health of the patient, and the severity of the injury. Causes Achilles tendon rupture occurs in people that engage in strenuous activity, who are usually sedentary and have weakened tendons, or in people who have had previous chronic injury to their Achilles tendons. Previous injury to the tendon can be caused by overuse, improper stretching habits, worn-out or improperly fitting shoes, or poor biomechanics (flat-feet). The risk of tendon rupture is also increased with the use of quinolone antibiotics (e.g. ciprofloxacin, Levaquin). Symptoms Although it's possible to have no signs or symptoms with an Achilles tendon rupture, most people experience pain, possibly severe, and swelling near your heel. An inability to bend your foot downward or "push off" the injured leg when you walk. An inability to stand up on your toes on the injured leg. A popping or snapping sound when the injury occurs. Seek medical advice immediately if you feel a pop or snap in your heel, especially if you can't walk properly afterward. Diagnosis A typical history as detailed above together with positive clinical examination usually will clinch the diagnosis. In an acute rupture, one can usually feel the gap in the tendon from the rupture. There may be swelling or bruising around the ankle and foot of the injured leg. With the patient lying on the tummy (prone position) with the knee flexed, the examiner should see the ankle and foot flex downwards (plantarward) when squeezing the calf muscles. If there is no movement in the ankle and foot on squeezing the calf muscle, this implies that the calf muscle is no longer attached to the heel bone due to a complete Achilles tendon rupture. Non Surgical Treatment Once the Achilles tendon is partially damaged, one should exercise great care. The risk of rupture is high and if pain is associated with walking, one should consult with an orthopedic surgeon or a sports physician. A complete rupture of the Achilles tendon is never treated at home. It is important to understand that there are no minerals, nutrients, or herbs to treat Achilles tendon injury and any delay just worsens the recovery.  Surgical Treatment Surgical techniques for rupture repair are varied but usually involve reapproximation of the torn ends of the Achilles tendon, sometimes reinforced by the gastrocsoleus aponeurosis or plantaris tendon. Open reconstruction is undertaken using a medial longitudinal approach. Studies indicate that patients who undergo percutaneous, rather than an open, Achilles tendon rupture repair have a minimal rate of infection but a high rate of sural nerve entrapment (16.7% of treated cases). Prevention The following can significantly reduce the risk of Achilles tendon rupture. Adequate stretching and warming up prior to exercising. If playing a seasonal sport, undertake preparatory exercises to build strength and endurance before the sporting season commences. Maintain a healthy body weight. This will reduce the load on the tendon and muscles. Use footwear appropriate for the sport or exercise being undertaken. Exercise within fitness limits and follow a sensible exercise programme. Increase exercise gradually and avoid unfamiliar strenuous exercise. Gradual ?warm down? after exercising.
Surgical Treatment Surgical techniques for rupture repair are varied but usually involve reapproximation of the torn ends of the Achilles tendon, sometimes reinforced by the gastrocsoleus aponeurosis or plantaris tendon. Open reconstruction is undertaken using a medial longitudinal approach. Studies indicate that patients who undergo percutaneous, rather than an open, Achilles tendon rupture repair have a minimal rate of infection but a high rate of sural nerve entrapment (16.7% of treated cases). Prevention The following can significantly reduce the risk of Achilles tendon rupture. Adequate stretching and warming up prior to exercising. If playing a seasonal sport, undertake preparatory exercises to build strength and endurance before the sporting season commences. Maintain a healthy body weight. This will reduce the load on the tendon and muscles. Use footwear appropriate for the sport or exercise being undertaken. Exercise within fitness limits and follow a sensible exercise programme. Increase exercise gradually and avoid unfamiliar strenuous exercise. Gradual ?warm down? after exercising.
 The Achilles tendon is the largest and most vulnerable tendon in the body. It joins the gastrocnemius (calf) and the soleus muscles of the lower leg to heel of the foot. The gastrocnemius muscle crosses the knee, the ankle, and the subtalar joints and can create stress and tension in the Achilles tendon . Tendons are strong, but not very flexible so they can only so far before they get inflammed and tear or rupture.
The Achilles tendon is the largest and most vulnerable tendon in the body. It joins the gastrocnemius (calf) and the soleus muscles of the lower leg to heel of the foot. The gastrocnemius muscle crosses the knee, the ankle, and the subtalar joints and can create stress and tension in the Achilles tendon . Tendons are strong, but not very flexible so they can only so far before they get inflammed and tear or rupture.